Envis Centre, Ministry of Environment & Forest, Govt. of India
Printed Date: Thursday, September 18, 2025
Nipah Virus
Nipah Virus(NiV):
Nipah virus (NiV) is a member of the family Paramyxoviridae, genus Henipavirus. Its name originated from Sungai Nipah, a village in the Malaysian Peninsula where pig farmers became ill with encephalitis. Nipah was first identified in Malaysia in 1998. In India the disease was first reported in 2001(Siliguri, West Bengal) and again six years later (2007) (Nadia,West Bengal) with the two outbreaks claiming 50 lives. In India the NiV cases observed from person-to-person transmission in hospital settings (nosocomial transmission). In 2001, NiV was again identified as the causative agent in an outbreak of human disease occurring in Bangladesh. Genetic sequencing confirmed this virus as Nipah virus, but a strain different from the one identified in 1999. Unlike the Malaysian NiV outbreak, outbreaks occur almost annually in Bangladesh and have been reported several times in India.
In order to stop the outbreak, more than a million pigs were euthanized, causing tremendous trade loss for Malaysia. Since this outbreak, no subsequent cases (in neither swine nor human) have been reported in either Malaysia or Singapore
Nipah virus (NiV) infection is a newly emerging zoonosis that causes severe disease in both animals and humans. The natural host of the virus is fruit bats of the Pteropodidae family, Pteropus genus.
Nipah induces flu-like symptoms that often lead to encephalitis and coma. Fruit bats are considered as the main carrier of the virus for which there is no vaccination, according to the World Health Organization.
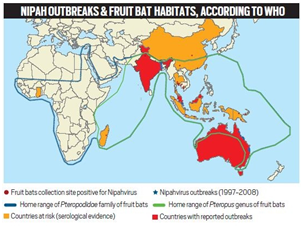
Source: WHO
Transmission:
Nipah virus infection in humans has a range of clinical presentations, from asymptomatic infection to acute respiratory syndrome and fatal encephalitis. Bats shed the virus in their excrement and secretions, but they are symptomless carriers. NiV is highly contagious among pigs and is spread by coughing.
During the initial outbreaks in Malaysia and Singapore, most human infections resulted from direct contact with sick pigs or their contaminated tissues. Transmission is thought to have occurred via respiratory droplets, contact with throat or nasal secretions from the pigs, or contact with the tissue of sick animals.
While the outbreak in Malaysia had progressed from the natural host (fruit bats), to amplification host (livestock) and finally to humans, in Bangladesh no amplification host was needed. The virus has also been isolated from environmental samples of bat urine and partially eaten fruit in Malaysia. Due to the migratory habit of the locally abundant fruit bats in South Asia, Nipah outbreaks occur more in this region People were somehow being directly infected by fruit bats. In Bangladesh and India the outbreaks due to consumption of fruits or fruit products (e.g. raw date palm sap) contaminated with urine or saliva from infected fruit bats was the most likely source of infection. Other people seem to have been infected while working in the trees.
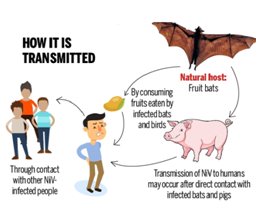
Transmission of Nipah virus
Source:http://www.homeopathicmedicine.info/en/medicine-for-nipah-virus-infection/
Signs and symptoms:
Human infections range from asymptomatic infection, acute respiratory infection (mild, severe), and fatal encephalitis. Infected people initially develop influenza-like symptoms of fever, headaches, myalgia (muscle pain), vomiting and sore throat. This can be followed by dizziness, drowsiness, altered consciousness, and neurological signs that indicate acute encephalitis. Some people can also experience atypical pneumonia and severe respiratory problems, including acute respiratory distress. Encephalitis and seizures occur in severe cases, progressing to coma within 24 to 48 hours.
The incubation period (interval from infection to the onset of symptoms) is believed to range between from 4-14 days. However an incubation period as long as 45 days has been reported.
Long-term sequelae following Nipah virus infection have been noted, including persistent convulsions and personality changes. Latent infections with subsequent reactivation of Nipah virus and death have also been reported months and even years after exposure.
Diagnosis:
Laboratory diagnosis of a patient with a clinical history of NiV can be made during the acute and convalescent phases of the disease by using a combination of tests. Virus isolation attempts and real time polymerase chain reaction (RT-PCR) from throat and nasal swabs, cerebrospinal fluid, urine, and blood should be performed in the early stages of disease. Antibody detection by ELISA (IgG and IgM) can be used later on. In fatal cases, immune histochemistry on tissues collected during autopsy may be the only way to confirm a diagnosis.
Treatment:
NiV infection in humans has a range of effects, from asymptomatic infection to acute respiratory distress syndrome and fatal encephalitis. The primary treatment is intensive supportive care. Treatment is focused on managing fever and the neurological symptoms. Ribavirin may alleviate the symptoms of nausea, vomiting, and convulsions.
There are currently no antiviral drugs or vaccines available to treat Nipah virus infection for either people or animals. Intensive supportive care with treatment of symptoms is the main approach to managing the infection in people. Experimentally, the therapeutic use of a neutralizing human monoclonal antibody, the m102.4, which recognizes the receptor binding domain of the NiV G glycoproteins, appeared promising in a ferret animal model. Furthermore, the m102.4 was also successfully tested in Non Human Primate (NHP) models against challenge with related Hendra virus.
Prevention:
Currently, there are no vaccines for both humans and animals. Intensive supportive care is given to humans infected by Nipah virus. Strategies include preventing farm animals from eating fruit contaminated by bats and avoiding consumption of contaminated date palm sap. According to WHO, ribavarin can reduce the symptoms of nausea, vomiting, and convulsions associated with the disease. Individuals infected need to be hospitalised and isolated. Special care should be taken to prevent human-to-human transmission. Surveillance systems should be established to detect the virus quickly and to initiate appropriate control measures. Healthcare workers caring for patients should put in place standard precautions including washing hands. Wearing a gown, mask, cap and gloves is also recommended.
Source:
https://www.livemint.com/Science/tGl90B7ezrazdy6jG1GoJN/What-is-Nipah-virus-and-how-is-it-transmitted.html
https://economictimes.indiatimes.com/news/politics-and-nation/all-about-nipah-the-virus-that-has-entire-kerala-in-panic-mode/articleshow/64258031.cms
http://www.thehindu.com/sci-tech/science/all-you-need-to-know-about-nipah-virus/article23950533.ece
https://www.omicsonline.org/open-access/nipah-virus-2329-9088.1000129.php?aid=16706
http://www.who.int/news-room/fact-sheets/detail/nipah-virus
https://www.cdc.gov/vhf/nipah/symptoms/index.html