More About Malaria
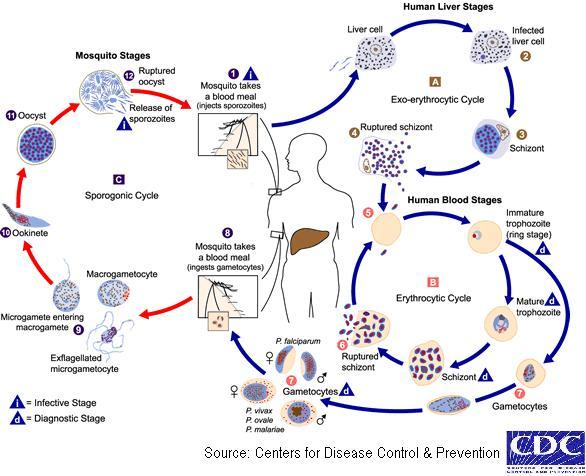
Malaria has probably influenced to a great extent human populations and human history. It is a disease, which can be transmitted to people of all ages. It is caused by parasites of the species plasmodium that are spread from person to person through the bites of infected mosquitoes.
Species and Distribution
P. malariae, P. vivax, P. falciparum and P. ovale are the most important types affecting man. The other species are primarily parasites of other mammals, affecting man only rarely and not seriously.
3 subtypes of P. vivax have been reported: Two variants of the circumsporozoite protein of P. vivax (VK210 and VK247) have been identified and recently, a putative third CS variant of P. vivax, referred to as causing P. vivax-like malaria has been reported
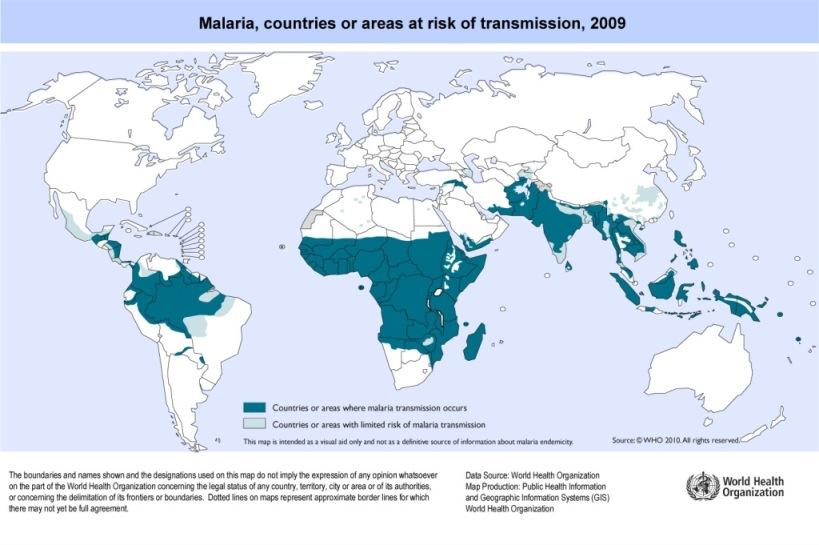
P. vivax is the commonest cause of human malaria in Central America, North Africa, southern and western Asia. P. falciparum is the predominant species in Africa, New Guinea and Haiti. Both P. vivax and P. falciparum are found in South America, other parts of Asia and Oceania. P. falciparum is the cause for all mortality and most of the morbidity due to malaria. P. ovale is restricted to western Africa. P. malariae is probably more wide spread than as made out to be in only a few pockets here and there.
Transmission
Malaria is transmitted from man to man by the female anopheles mosquito, one of the most capable vectors of human disease. Various species have been found to be the vectors in different parts of the world. A. gambiae complex is the chief vector in Africa and A. freeborni in N. America. Nearly 45 species of the mosquito have been found in India and A. culicifacies, A. fluviatilis, A. minimus, A. philippinensis, A. stephensi, A. sundaicus, and A. leucosphyrus have been implicated in the transmission of malaria. A. fluviatilis, A. minimus are found in the foot-hill regions, A. stephensi, A. sundaicus are found in the coastal regions, A. culicifacies and A. philippinensis are found in the plains. Species like A. stephensi are highly adaptable and are found to be very potent vectors of human malaria.
Epidemiology:
Malaria is transmitted in large areas of Africa, Central and South America, the island of Hispaniola (includes Haiti, Jamaica and the Dominican Republic), Asia (including the Indian subcontinent, Southeast Asia and the Middle East), Eastern Europe, and the South Pacific. Malaria affects more than 2400 million people, over 40% of the world's population, in more than 100 countries in the tropics from South America to the Indian peninsula. The tropics provide ideal breeding and living conditions for the anopheles mosquito, and hence this distribution. Every year 300 million to 500 million people suffer from this disease (90% of them in sub-Saharan Africa, two thirds of the remaining cases occur in six countries- India, Brazil, Sri Lanka, Vietnam, Colombia and Solomon Islands). WHO forecasts a 16% growth in malaria cases annually. About 1.5 million to 3 million people die of malaria every year (85% of these occur in Africa), accounting for about 4-5% of all fatalities in the world. About 40% of the world’s population, mostly those living in the poorest countries, are at risk of malaria. Early diagnosis and prompt treatment are two basic elements of malaria control.
Treatment:
Early and effective treatment of malaria can shorten the duration of the infection and prevent further complications including the great majority of deaths. Access to disease management should be seen not only as a component of malaria control but a fundamental right of all populations at risk.
Inappropriate use of antimalarial drugs in the past century contributed to widespread resistance in the malaria parasite to drugs such as chloroquine, leading to rising rates of sickness and death. Over the past decade, a new group of antimalarials – known as artemisinin-based combination therapies – has brought new hope in the fight against malaria.
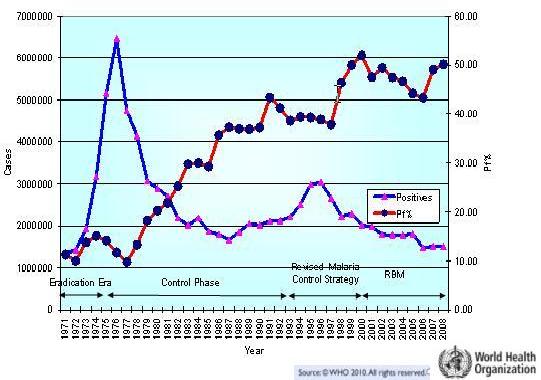
Global scenario: Malaria cases in India: 1971-2008
Clinical Symptoms :
Clinical manifestations
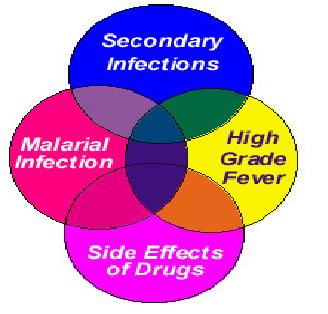
Symptoms of malaria include atypical fever, headache, body ache, backache and joint pains, Dizziness, vertigo, Altered behaviour, acute psychosis, Altered sensorium, Convulsions, coma, Breathlessness, Chest pain, Acute abdomen, Weakness, Vomiting and diarrhoea, Jaundice, Pallor, Puffiness of lids, Secondary infections, Hepatosplenomegaly etc.
Severe malaria can progress extremely rapidly and cause death within hours or days. In the most severe cases of the disease, fatality rates can exceed 20%, even with intensive care and treatment. In endemic areas, treatment is often less satisfactory and the overall fatality rate for all cases of malaria can be as high as one in ten. Over the longer term, developmental impairments have been documented in children who have suffered episodes of severe malaria.
Vector Control :
The main objective of malaria vector control is to significantly reduce the rate and number of cases of both parasite infection and clinical malaria. This is achieved by controlling the malaria-bearing mosquito and thereby reducing or interrupting transmission.
Long-lasting insecticidal nets can be used to provide protection to risk groups, especially young children and pregnant women in high transmission areas. This provides personal protection. The nets can also protect communities when coverage is high enough (more than 80% of people in a target community sleeping inside them). Indoor residual spraying is the most effective means of rapidly reducing mosquito density. Its full potential is obtained when at least 80 % of premises with malaria vectors are sprayed.
Pregnant women are at high risk not only of dying from the complications of severe malaria, but also spontaneous abortion, premature delivery or stillbirth. Malaria is also a cause of severe maternal anaemia and is responsible for about one third of preventable low birth weight babies. It contributes to the deaths of an estimated 10 000 pregnant women and up to 200 000 infants each year in Africa alone.
Economic burden
Malaria is estimated to cause 300- 500 million clinical cases and over one million deaths each year. Malaria causes an average loss of 1.3% of annual economic growth in countries with intense transmission. It traps families and communities in a downward spiral of poverty, disproportionately affecting marginalized and poor people who cannot afford treatment or who have limited access to health care. Malaria has lifelong effects through increased poverty and impaired learning. However, it is preventable and curable.
- Malaria ranks third among the major infectious diseases in causing deaths- after pneumococcal acute respiratory infections and tuberculosis. It is expected that by the turn of the century malaria would be the number one infectious killer disease in the world.
- It accounts for 2.6 percent of the total disease burden of the world. It is responsible for the loss of more than 35 million disability-adjusted life-years each year.
- Estimated annual expenditure on malaria research, prevention and treatment: $ 84 million.
- Estimated worldwide expenditure per malaria fatality: $ 65; as compared to $ 3274 for HIV/AIDS and $ 789 for asthma. That is to say, one HIV/AIDS death is equal to about 50 malaria deaths.
Reasons for resurgence
Malaria was nearly eradicated from most parts of the world by the early 60's, owing largely to concerted anti malarial campaigns world over under the guidance of the World Health Organization.
The following are some of the reasons for the resurgence of malaria:
| Man made |
Complacency and laxity in anti malarial campaigns; conflicts and wars; migrations; deteriorating health systems; poverty |
| Parasite |
Drug Resistance |
| Vector |
Insecticide Resistance and ban on DDT |
| Environment |
Global Warming - increased breeding and life span of the insect vector |
| Jet Age |
Shrinking World - spread of malaria from endemic areas to all other parts of the world |
Achievements and Initiatives in India:
- Incidence of malaria has been brought down below 2 million cases annually since 2002 and sustained near 1.5 million in recent years
- 12 million fever cases tested for malaria with RDT
- Nearly 95% of Pf cases are treated with ACT
- Procurement of LLINs initiated in the country & 1.3 million LLINs distributed in 2009
- 170,000 ASHAs (Community based services providers) trained on malaria diagnosis & treatment
- 1-2 Sentinel sites identified for assessing the burden of severe malaria and case fatality
- Improved surveillance and supervision by providing additional 3500 MPWs and 300 MTS respectively
Issues and challenges:
- The constraints impending the progress include insecticide resistance in A. culicifacies and A. stephensi, the major rural and urban vectors obtaining in the country, and exophily and exophagyin A. dirus, A. minimum and A. fluviatilis in the wet climatic zones.
- The drug resistance of P. falciparum to chloroquine is widespread. However for SP(Sulfadoxine-Pyrimethamine based combinations) , low to moderate level resistance is observed in north-east states, in kolar district in Karnataka, and one district each in Madhya Pradesh and West Bengal respectively. Quinine resistance is limited to few places of North-East states only.
- Problem of urban malaria is one of major hurdle for malaria control programme.
- Also, scarcity of funds, man made malariogenic condition by various development projects, transmigration are other main problems in malaria control programme.
- Difficulty in regular malaria surveillance activities due to difficult terrain conditions like hills and forests poses many problems.
- Vacancy of key positions of programme in the states
- Frequent shifting of various programme officers at states, zonal and country level.
- Inadequacy of transports affecting supervision of operational activities.
Sources:
http://www.searo.who.int/EN/Section10/Section21/Section340_4027.htm
http://www.malariasite.com
http://highered.mcgrawhill.com/sites/0072437316/student_view0/chapter28/animations.html
http://www.malaria.com/info/malaria-prevention-control.php